Bacterial virulence factors are aspects of the bacterium that influence its interaction with host cells. These factors can influence adhesion, colonization, invasion, tissue damage, evasion of the immune system, acquisition of nutrients, spread of the bacterium and many other aspects of the bacteria’s life within an animal. All of these virulence factors are encoded by virulence genes, which ultimately determine the pathogenicity of certain bacterial species or strains.
Adhesion and Colonization
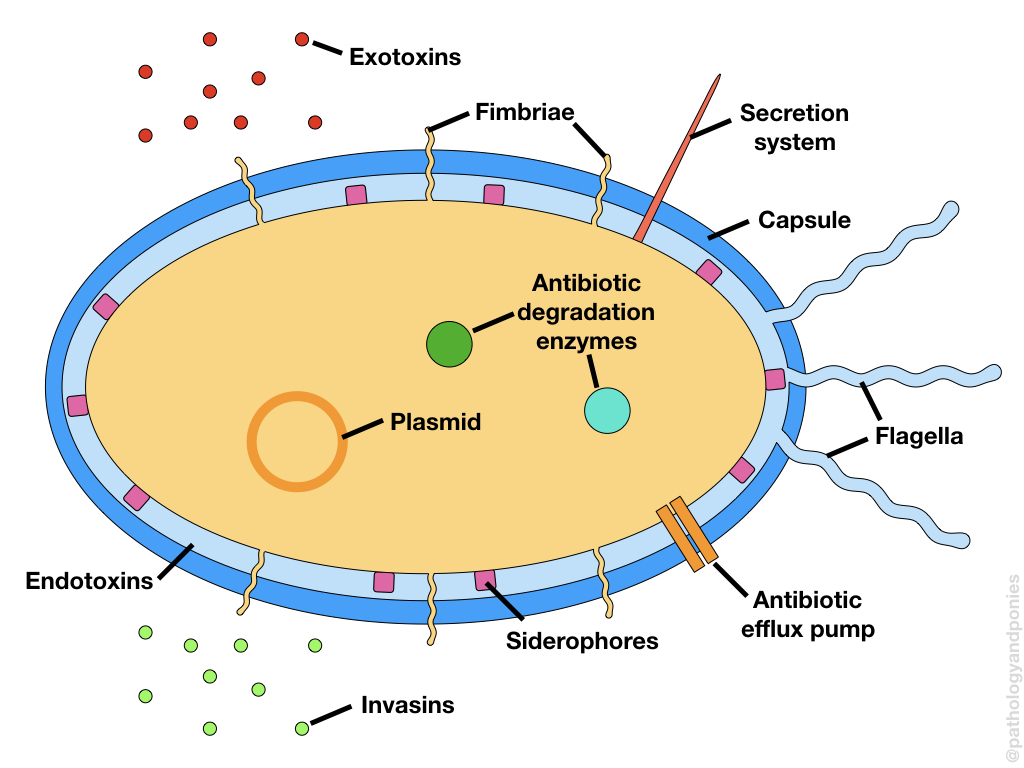
Adhesion factors allow the bacteria to attach to cells, which is the first critical step in producing an infection. The majority of these factors are grouped under adhesins, which are membrane proteins that attach to a specific receptor on host cells. Some bacteria have characteristic long extensions of their cell membrane called pili or fimbriae. Typically, these extensions are used in motility, however they are also coated in adhesins and can act as an attachment point for the bacterium. Other bacteria produce a sticky capsule around their cell wall, which can also help attach them to a surface. Attachment of large numbers of bacteria allows a colony to form, which triggers bacteria to produce other virulence factors that enhance infection.
Some bacteria form biofilms as part of their colonization process, which are large aggregates of bacteria in a polysaccharide matrix. Biofilms make bacteria resistant to phagocytosis and some types of antibiotics, improving their pathogenicity.
Colonization may require additional nutrients that the bacteria needs to extract from the host. The best example of this is iron, which is usually bound to proteins like heme or ferritin within the host. To access iron, some bacteria produce siderophores, which stimulate release of iron from these carrier proteins to make it accessible for the bacterium.
Invasion Factors
The main purpose of invasion factors is to increase the spread of the bacteria throughout the host. The major category of these factors are invasins. Most invasins are enzymes directed against normal host defenses, such as mucosae and the extracellular matrix. Some invasins may also target cells themselves, such as proteases (destroy proteins), DNases (destroy DNA) and lysins (form pores in cells). Through these enzymes, the bacteria is able to carve out a home for itself within the tissue, and gain access to important body “highways” like the blood vessels and lymphatics.
Evasion Factors
Once a bacterium has entered a host, it is up against a strong challenger: the immune system. So, many bacteria have evolved methods of evading the immune system. The most common evasion factor is developing a capsule, which helps prevent phagocytosis and immune recognition. Some bacteria produce proteins that specifically disrupt phagosome-lysosome fusion, allowing them to escape normal phagocytic destruction. Finally, some bacteria produce immunoglobulin proteases, allowing them to avoid destruction by the adaptive immune system.
Bacterial Toxins
Bacterial toxins are probably the most significant virulence factors produced, as their primary role is disrupting cell function or causing cell death. There are several different types of toxins, with different mechanisms of action. The five most common mechanisms are outlined below.
| Mechanism | Pathogenesis |
|---|---|
| Enzymatic lysis | Usually phospholipases which destroy cell membranes |
| Pore formation | Disrupts the cell membrane to form a pore, allowing leakage of cellular contents |
| Inhibiting protein synthesis | Prevents the cell from producing new proteins, leading to cell death |
| Dysfunction of ion pumps | Increases the activity of ion and water pumps, causing loss of water and electrolytes from cells |
| Disruption of SNARE proteins | Prevents vesicles from fusing with the cell membrane, preventing release of important cellular proteins |
Bacterial toxins come in three major types: exotoxins, endotoxins and A-B toxins.
| Type | Delivery Method |
|---|---|
| Exotoxins | Secreted externally into the environment or into cells via secretion systems (needle-like structures that pierce target cell membranes) |
| Endotoxin | Component of the bacterial wall that is released when the bacterium dies |
| A-B toxin | B portion of toxin binds to cell and facilitates delivery of A portion of toxin into the cell |
Antibiotic Resistance
Although not purely related to pathology, antibiotic resistance factors are also important to mention. Bacteria have four main mechanisms of antibiotic resistance:
- Enzymatic deactivation
- Altering the typical binding site for the antibiotic
- Altering the metabolic pathway involved in processing the antibiotic
- Pumping the antibiotic out of the cell to prevent its effects
Like other virulence factors, these antibiotic resistance mechanisms are encoded by virulence genes.
Engleberg NC, DiRita V, Dermody TS. Schaechter’s Mechanisms of Microbial Disease, Fifth Edition. Lippincott Williams & Wilkins 2012.
Kumar V, Abbas AK, Aster JC. Robbins and Cotran Pathologic Basis of Disease, Tenth Edition.
Zachary JF. Pathologic Basis of Veterinary Disease, Sixth Edition.