We’ve hit 1500 followers on Facebook! 🎉 This week’s posts will be all about how different kinds of pathogens (disease-causing agents) actually cause disease. Today’s post is on bacterial infections!
What are bacteria? Why are some infectious?
Bacteria are single-celled organisms that were probably one of the first life forms to appear on Earth. Bacteria are found everywhere, and not all of them cause disease. However, some bacteria rely on a host to survive, meaning that they need to develop ways to infect their host (e.g. an animal), evade the immune system and then spread to another host. These are the types of bacteria we will focus on today!
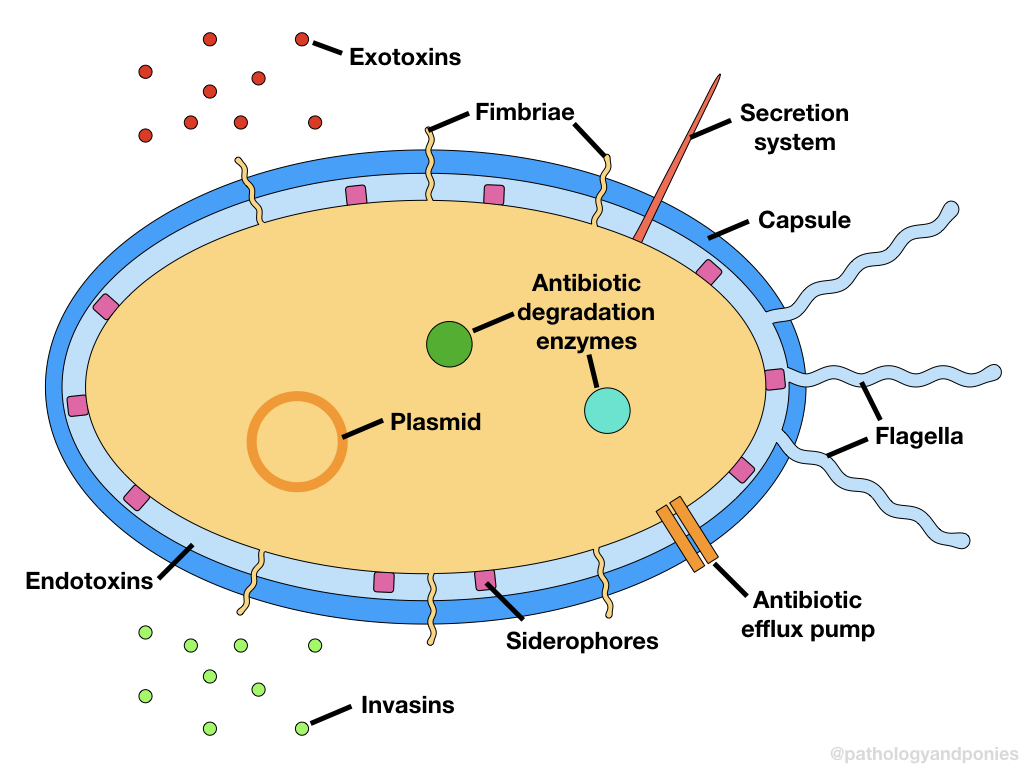
To carry out these functions, infectious bacteria produce virulence factors, which are products or structures that increase the pathogenicity (ability to cause disease) of the bacteria. The genetic code for virulence factors are found on plasmids, loops of genetic material that can be passed between bacteria. There are three basic categories of virulence factors: adhesion factors, invasion factors and toxins. All of these factors are derived from bacterial proteins, and have different specialized functions to aid in bacterial survival.
How do bacteria attach to cells?
As mentioned, one of the first things a bacteria needs to do is infect their host. In order to do so, the bacteria must attach itself to a host cell at the site of entry, so that it can establish an infection. The virulence factors that allow bacteria to do this are called adhesins, and are generally proteins embedded onto the cell surface that interact with host cells.
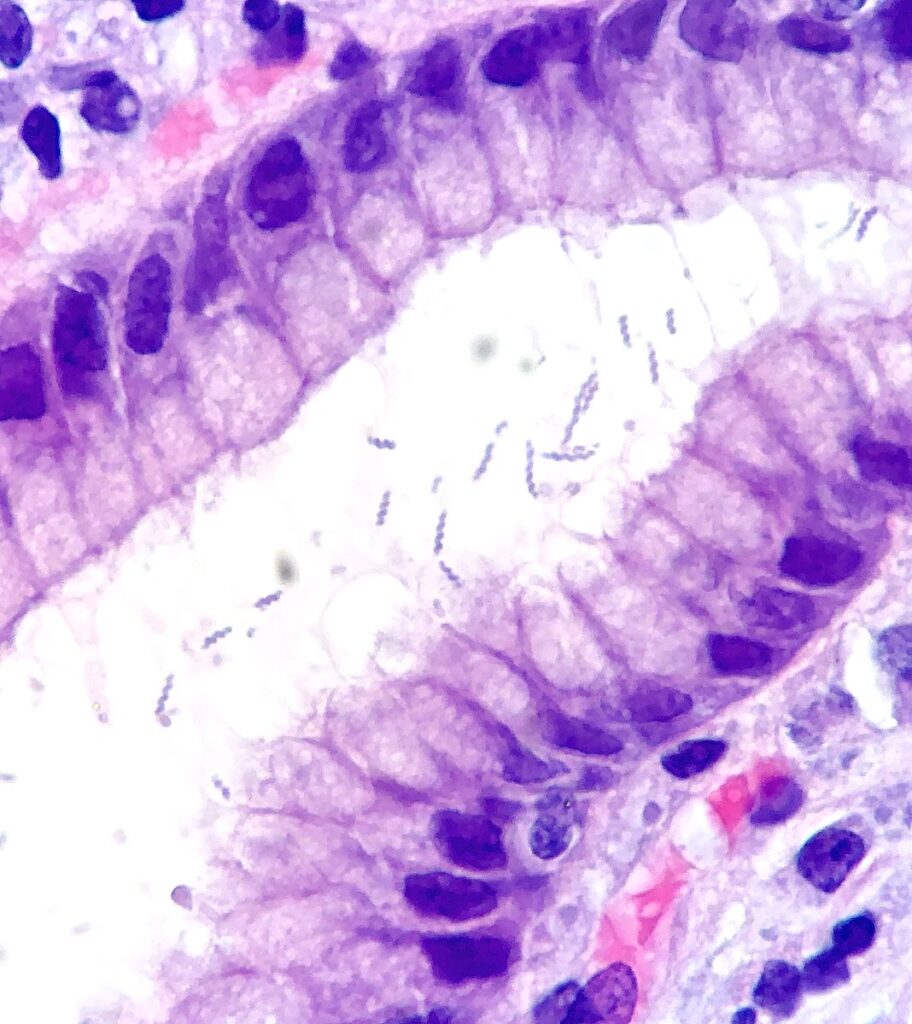
One of the most common types of adhesins are fimbriae, which are long, finger-like projections off of the bacteria. These fingers latch onto the host cell, and give the bacteria the opportunity to form a colony, basically a bunch of bacteria attached to a single cell. This process of colonization is what ultimately sets the stage for invasion.
Another defense mechanism the body has against bacterial attachment is binding iron to proteins to prevent bacteria from using it. Some types of bacteria need extra iron to sustain their colonies, as it is a critical nutrient for bacterial survival. So, these bacteria have developed proteins called siderophores, which specifically counteract the body’s mechanisms of iron storage, so that more iron is accessible to the bacteria. Neat!
How do bacteria invade into a host?
After forming a colony, the bacteria work together to allow for entry into the host. They do this by producing enzymes called invasins. These enzymes specifically target the normal defenses of the host cells. For example, some bacteria produce collagenase, an enzyme which breaks down structural collagen on mucosal surfaces. Some may also produce proteinases (break down protein), lipases (break down fat) and DNases (break down DNA) which cause death of the cells they are attached to.
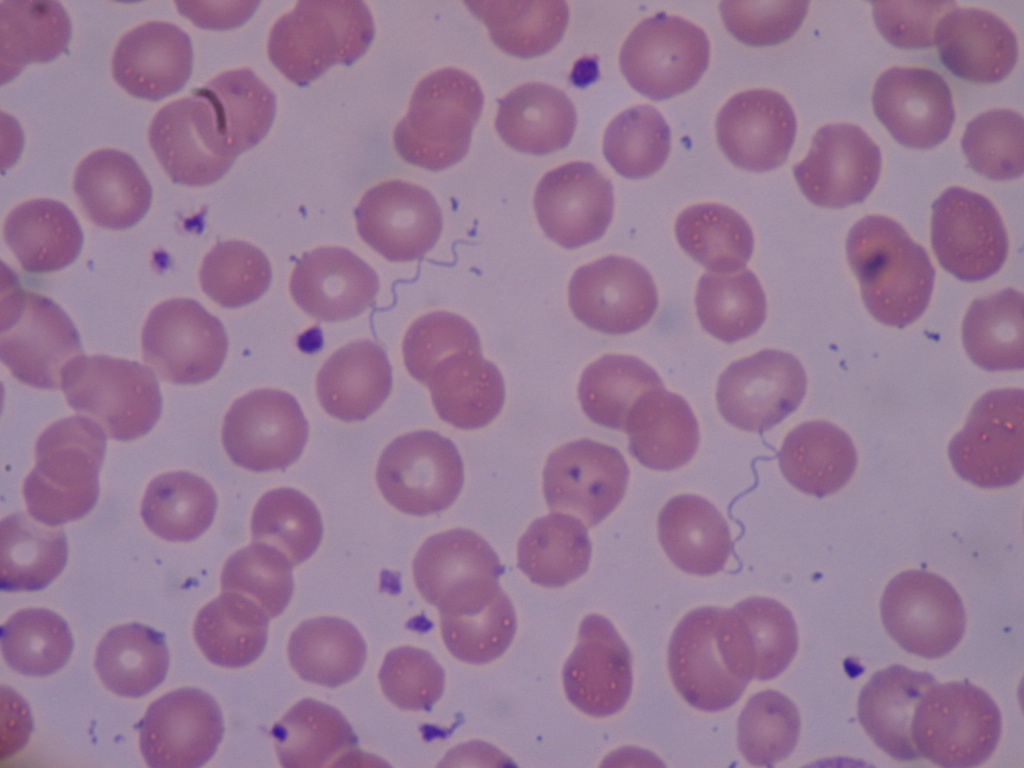
Ultimately, breaking down the cells at the site of entry gives the bacteria access to important “highways” like the bloodstream, lymphatic system or even nerves. From there, the bacteria can spread to its preferred home, where it will grow best.
How do bacteria evade the immune system?
Bacteria are up against a huge challenge once they enter the host: the host’s immune system. However, through natural selection and a lot of time, bacteria have developed ways to protect themselves against this challenger. Some examples of this include having a capsule which prevents the bacterium from being recognized as an invader by the immune system, or prevents the immune system from attaching to the bacterium to allow its destruction. Others produce enzymes that specifically target immune system cells or components. For example, some bacteria produce immunoglobulin proteases, which break down any antibodies that form against the bacteria. Wild!
How do bacteria cause disease?
The main way that bacteria cause disease is through production of toxins. Now, it might seem counterintuitive for something that needs a host to survive to cause disease in that host! However, the disease that the bacteria produces often benefits that bacteria, either by causing tissue destruction to allow access to a new area of the body to colonize, or causing clinical signs that allow the bacteria to spread to a new host. The two main types of toxins are endotoxin and exotoxin, although many bacteria produce their own specialized toxins as well.
Exotoxins are toxins that are secreted from the bacteria, and they usually are involved in cell killing. These toxins usually bind to a host cell and form a pore (hole) in the cell membrane. Cells use their cell membrane to produce a concentration gradient between the inside of the cell and the outside world, which they can harness for things like producing energy. With the cell membrane disrupted, this concentration gradient is removed, and the cell ultimately dies. Another type of exotoxin called lipoteichoic acid actually activates the immune system, which again may seem counterintuitive. However, the activated immune system releases tons of destructive enzymes in an attempt to kill the invader, which often results in destruction of host cells too. Bacteria with lipoteichoic acid use this destructive property of the immune system to their benefit, as it does the bacteria’s work for it!
Endotoxins are actually a component of the bacteria itself, and are released when the bacteria dies. The main endotoxin is lipopolysaccharide (LPS), which is a sugar complex found in the bacterial cell wall. LPS is actually toxic to most host cells, and causes widespread tissue damage wherever it is released. If it is released into the bloodstream, you can imagine how much destruction it can cause! This is called toxic shock syndrome. Endotoxins are basically another way by which bacteria use the immune system to their advantage: if the immune system successfully kills a bacteria, suddenly a cascade of tissue damage is started that allows the bacteria to set up a lovely home!
How do bacteria evade antibiotics?
Thankfully we’ve discovered drugs that help treat bacterial infections, called antibiotics. However, bacteria always seem to be one step ahead of us! They have also evolved virulence factors that cause antibiotic resistance, which is a hot topic in medical fields. There are a few main ways bacteria can do this:
- Inactivation of the antibiotic via an enzyme.
- Altering the sites where the antibiotic would normally bind, so it can no longer attach itself to the bacterium.
- Using a different method of nutrient production to avoid antibiotics who disrupt nutrient pathways.
- Pumping antibiotics out of the bacterium once they enter, so they can’t exert their effects.
Unfortunately, every time we use an antibiotic, we are actually helping them become better at evading our drugs. This is through natural selection, where bacteria that have slight changes in their structure or behaviour that favour survival will live on, continue to replicate and produce more bacteria. So even though 99% of the bacteria might die from our antibiotic use, it’s that 1% that is left who comes back stronger than ever! This is why it is so important to use appropriate antibiotics that can successfully kill the bacteria in question, and to take the antibiotic for an appropriate length of time to ensure that every last bacteria is eliminated. Consultation with medical professionals is absolutely critical whenever an antibiotic is used!
Fun photos!
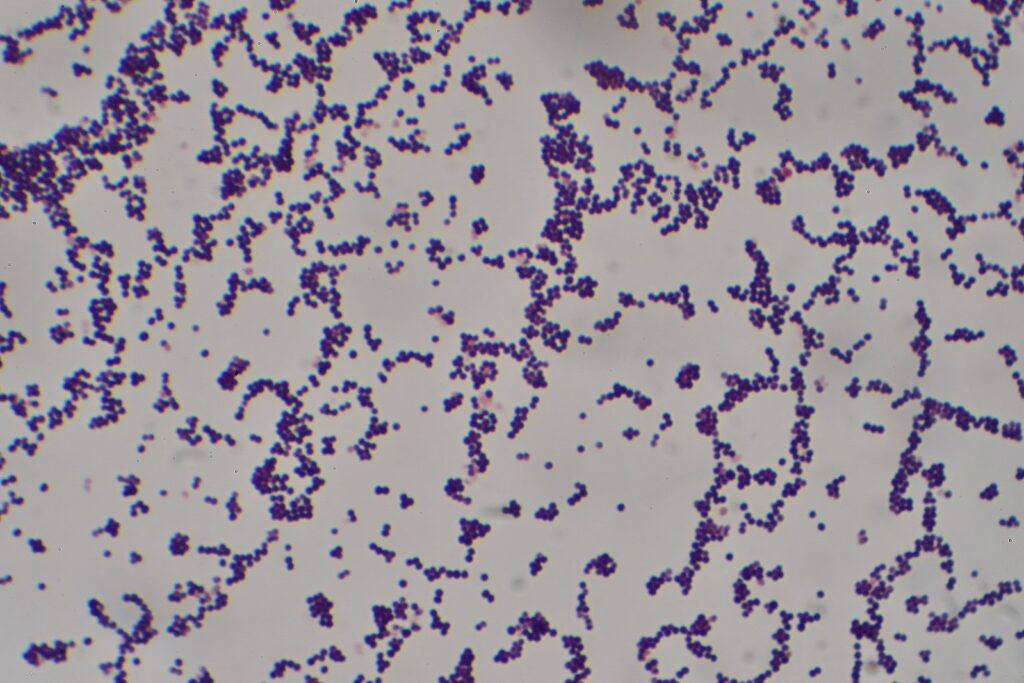
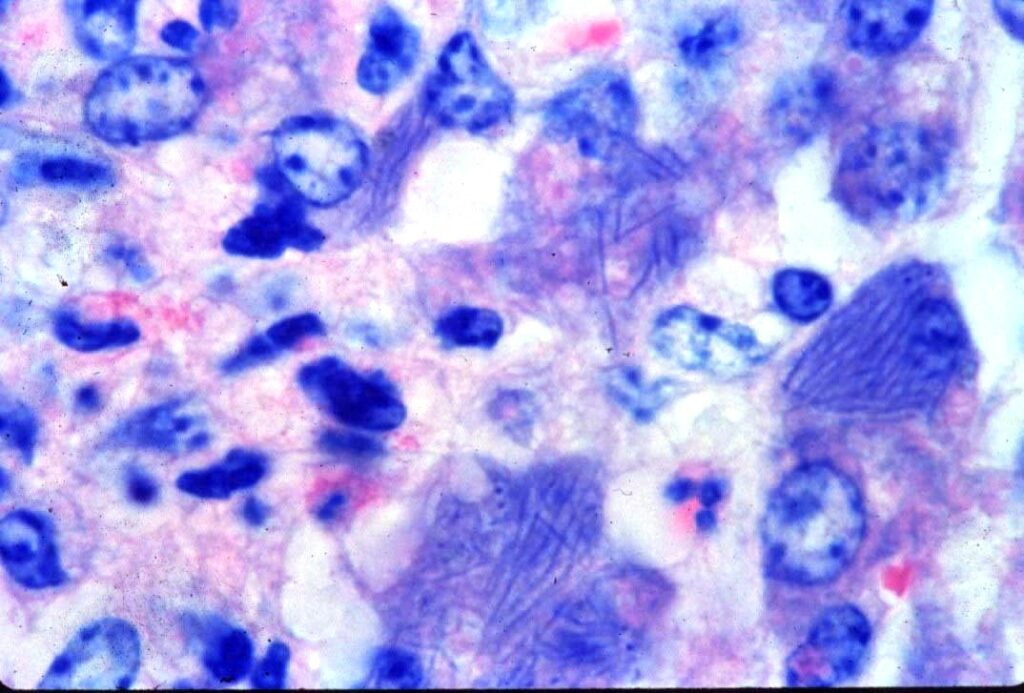
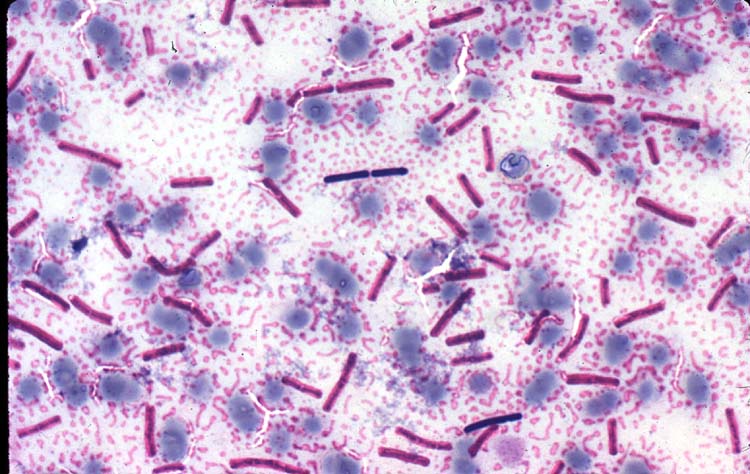
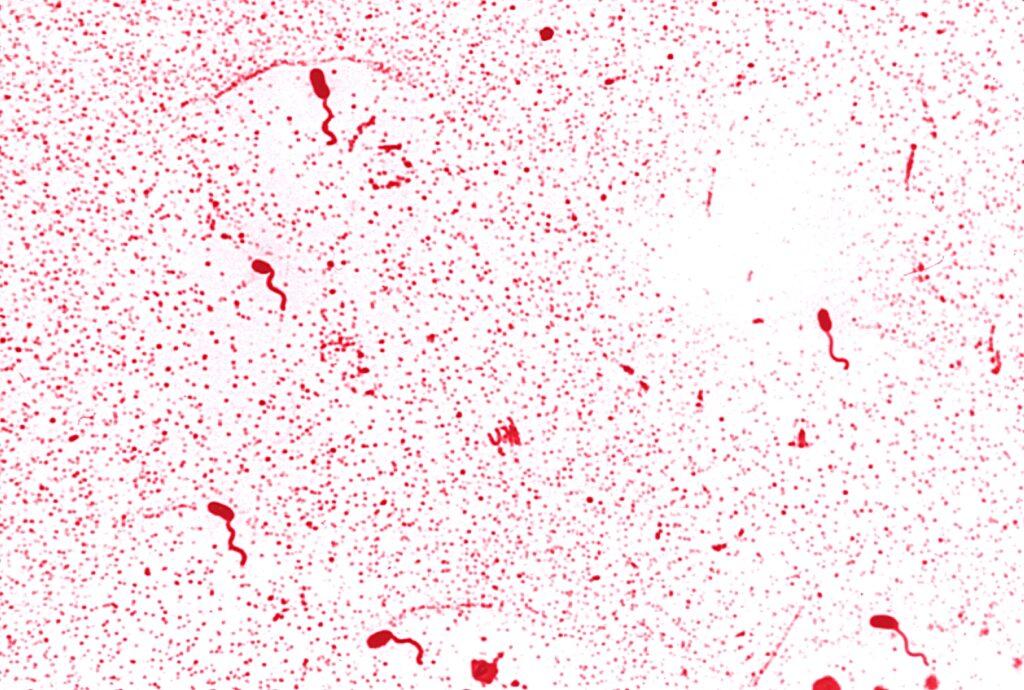
Bacteria actually come in lots of different shapes and structures! The main shapes are cocci (round), bacilli (rod-shaped), spirilla (spiral-shaped), vibrio (comma-shaped) and spirochaete (corkscrew-shaped). Some examples are included below.
Sources
Zachary JF. Pathologic Basis of Veterinary Disease, Sixth Edition.
Photos 1, 7 © Wikimedia Commons contributor Graham Beards, Bobjgalindo licensed under CC Share Alike 4.0 International.
Photos 3, 4 © Noah’s Arkive contributors King, Harrington licensed under CC BY-SA 4.0.
Photo 5 © Wikimedia Commons contributor Netha Hussain licensed under CC Share Alike 2.0 Generic.
Photo 6 © Center for Disease Control and Prevention.




